This article features text, audio, and video of a webinar hosted by Twill's Chairman, Dr. Andy Sekel, Ph.D. The program's title was “What Does 'Digital First' Mean for Behavioral Health and Can It Help Avoid The Mistakes of the Past?”
Dr. Sekel was joined by three panelists with exceptional insight into the health care industry.
Featured guests included Steve Blumenfield, head of Strategy and Innovation for Willis Towers Watson’s Health and Benefits business in North America; Dr. Stuart Lustig, Cigna’s National Medical Executive for Behavioral Health, and Michael Thompson, the President and CEO of the National Alliance of Healthcare Purchaser Coalitions.
The complete webinar is available here.
In this video clip, the panelists discuss how why they believe a digital-first approach to behavioral health care is essential.
Interview Excerpt Transcript
|
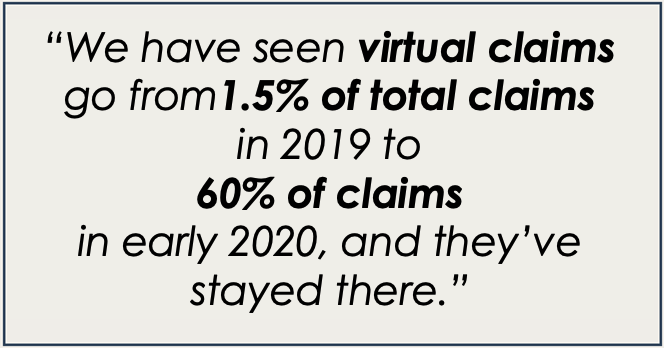
Steve Blumenfield: I'll start. I've been a big supporter of digital first as you've called it, but really what I'm supportive of and, and what we're seeing with our clients, is interest in looking for additional modalities that will try to get people to engage. We have an access problem in this country. There's no question about it. No matter how you slice it, you have an access to care problem. And sometimes that plays out in lots of ways. And we all know the challenges that members have trying to receive care, locate care. We need to find ways to make care available to anybody in any modality they want. It's got to be high quality. So, when I think digital first approach to behavioral health, as you described, it includes digital, app-based solutions. Web-based, it includes virtual care. It includes other ways outside of the nine-to-five office. Well, we saw from our surveys and we all know that anyone who practices in the mental health field saw during COVID that care didn't happen unless it was digitally virtually enabled. So, we've already seen that this works and our surveys found that the vast majority of people who tried virtual care actually found it was effective and would do it again. We also found that clinicians had similar experiences. So we're big supporters of trying to provide lots of different entry points for people to get care and people will want to take the ones most appropriate to them. And if those different entry points can do great navigation and be actual terrific solutions, then self-care is enabled as well as escalations to the right care at the right time. So that's maybe some opening thoughts. Right. Thank you. And let me talk about digital replacements discussions before we're really talking about software as well as tele-health. So all the different capabilities that are enabled by digital are part of the discussion. Stuart. You want to share your comments and then Michael. Dr. Stuart Lustig: Yeah, absolutely. When I think about my 20 plus years in the field of child psychiatry, and I think about some of the major changes that our field is undergone in recent decades, I would say that the shift to digital first is probably one of the most tectonically significant because it just impacts millions and millions of people. More so than anti-psychotics did when they first came out - the increased access of something that is infinitely scalable, like an app, or the efficiencies of something like a virtual treatment one-on-one because there were a greater efficiencies and fewer cancellations when you don't have to go across town to get to an appointment. I think the impact is really enormous and the pandemic has shown us that signal. I'll just say briefly and then turn it back over to you, Andy. We have seen virtual claims go from about one-and-a-half percent of our total claims in 2020 to 60% of claims in early 2020. And it's really kind of stayed there actually. So I think this is a really major shift that is not going away. Mike Thompson: And I'll just pile on a little bit. I don't think you're going to get as much disagreement as you might anticipate. We've had, as Steve said, serious problems in the system to be able to get access to care. And the care that's being provided is often provided either by primary care, without the support of people who are adequately trained in behavioral health, or by specialists who are. Doing it the way they always have without the benefits of technology and standardized measurement and follow through. And all of that has led to optimal access and some optimal quality in the system. Honestly, I can't envision a way for us to get to a scalable improved system with access for everyone if we aren't enabling it with a digital front end. And, and that can be whether it is an independent app with an artificial intelligence interface all the way to just being the front end to take assessment and then guide the care journey going forward. We know that if we have that more disciplined approach to mental health, we can catch things earlier, which means they will be less serious. They will be less expensive; we know there's a lot of interplay between mental health and every other condition. So doing that should be systematic with everybody who has a chronic condition and we also know that if we follow through and we reimagine using a disciplined approach to digital that outcomes are better by 20% to 60%. So I don't know how we move forward, unless we're thinking with a scalable approach to enforcing more discipline and earlier. |
If this interview was compelling for you, we invite you to watch the entire presentation here.
You May Also Like:
- An interview with Dr. Sekel: Where Mental Health Still Misses the Mark
- A letter from Twill's CEO: Connection is Healthcare