
Scientists have known for at least 30 years that behavioral and psychological factors influence our immune systems. If you ask people who work in healthcare whether the mind and body are connected, most will tell you that they are. Stop a person at random walking down the street and ask them if they have heard that stress can contribute to heart disease, and they are likely to tell you they have.
However, despite this widespread cursory understanding that the mind and body are linked, few understand exactly how, or the underlying physiological processes through which behavioral health treatment produces tangible improvements in physical health processes. This is the focus of psychoneuroimmunology.
Psychoneuroimmunology is the study of the interaction of psychology with the central nervous system, endocrine system, immune system and autonomic nervous system (both sympathetic and parasympathetic). While this field is relatively young compared to other medical and psychological areas, it offers critical insights into how the brain and body affect one another.
How stress harms our bodies
Stress-producing events can have profound effects on one’s susceptibility to illness and stress impacts a number of biological processes, including blood pressure, damage to muscle tissues, infertility, inhibition of growth, and inhibition of inflammatory responses1. Entire books have been written on this topic 2,3, but this article will present a high level overview.
The brain is the primary organ with the responsibility to interpret and regulate stress. While complex biological and chemical processes occur in the brain in response to perceived stress, a brief summary is that the hypothalamic-adrenal-pituitary (HPA) axis regulates neuroendocrine response to both internal and external stressors. In response to stressors, the hypothalamus secretes Corticotropin-Releasing Hormone (CRH or CRF) into the bloodstream, which signals the pituitary gland to release Adrenocorticotropic Hormone (ACTH).
ACTH travels down to the adrenal cortex and prompts the release of hormones such as cortisol. These hormones prepare the body to respond by increasing heart rate and sending blood to the heart, muscles, and organs. These hormones impact the autonomic nervous system broadly, including functions such as respiration rate, digestion, and cardiovascular function so that the body is primed to respond to the stressor(s).
In the short term, this stress response is an evolutionary tool to maximize survival, but in the long term, consistent and sustained stress causes hyperactivation of these mechanisms which can be damaging.
Chronic stress has become the new normal
Homeostasis is the process by which a living organism maintains a body’s state of optimal functioning through regulating biochemical and physiological processes to promote stability. Relatedly, allostasis, which literally means “achieving stability through change” is the process by which homeostasis is achieved.4 In other words, allostasis is the process by which a living organism responds to changes (including stressors) to achieve homeostasis.5
We know that on a daily basis, our internal biological environment is adapting in order to achieve and maintain equilibrium. Living in the 21st century means dealing with an abundance of stressors, many of which are relatively new phenomena—for example, pervasive social media use, the 24-hour news cycle, and other new circumstances that constantly bombard us with information we may perceive as stressful.
While allostatic load is adaptive and observed in anticipation of events that require biological systems to navigate successfully (e.g., changes in fat deposition in an animal preparing to hibernate) allostatic overload refers to a chronic state of distress. Over time, the cumulative adverse effects of our daily experiences and maladaptive health behaviors (e.g., disrupted sleep patterns, lack of exercise, unhealthy diet) exceed our threshold of what we are able to manage successfully and lead to allostatic overload, for which the consequences for mental and physical health can be severe.6
.png?width=1200&name=MOA-TL-Image-2%20(1).png)
When one considers the effect of chronic stress interacting with maladaptive health behaviors as listed above, as well as our bodies vigilantly working to return to homeostasis, it is no wonder that people are experiencing a myriad of physical and psychological syndromes. While millions of people suffering from depression and anxiety is not a new phenomenon, record rates have been reported globally recently.7,8,9 The COVID-19 pandemic has exacerbated this increase in rates, such that a recent review of literature found 28% and 26% jumps in rates of cases of major depressive disorder and anxiety disorders, respectively 10 and 54% said that COVID-19 has adversely impacted their mental health.11
How transformative healthcare helps us re-achieve balance
When one considers health in the context of psychoneuroimmunology, addressing mental and behavioral factors to improve patients’ functioning, symptoms, and quality of life makes good sense. Research has demonstrated that behavioral health intervention results in significant improvements across many conditions including arthritis, asthma, cancer, cardiovascular disease, chronic pain, diabetes, insomnia, obesity, pulmonary disease, substance use, cancer, and others. Further, having a comorbid mental illness is associated with healthcare costs that are twice as high 12 and it is estimated that about 30% of people with a chronic medical condition also have a mental health disorder.13
Two examples to illustrate the impact of behavioral health interventions on physical conditions:
Example #1: Asthma
Asthma is a condition in which airways become inflamed and breathing becomes difficult. At first pass one may wonder what behavioral health interventions can do for what seems to be an obviously physical disease. But having an asthma attack is a stressful event and as previously discussed, stress triggers a physical response that is designed to help us in the short-term but has long-term detriments.
Attacks are particularly aversive for asthma patients who also have anxiety disorders, because they reinforce avoidance behaviors (e.g., avoiding exercise due to breathing patterns that restrict air intake similar to an attack) and increase health-related fear or hypervigilance regarding threatening bodily symptoms. Individuals with asthma and anxiety, in turn, tend to over-perceive symptoms of asthma and overreact during asthma episodes, resulting in increased medication and healthcare use.14
The good news: Behavioral health treatment can lower health service utilization (hospitalization, ER visits, and GP visits), improve asthma symptoms and lung function, reduce absenteeism from work or school, and lead to better medication adherence.15
Example #2: Migraine
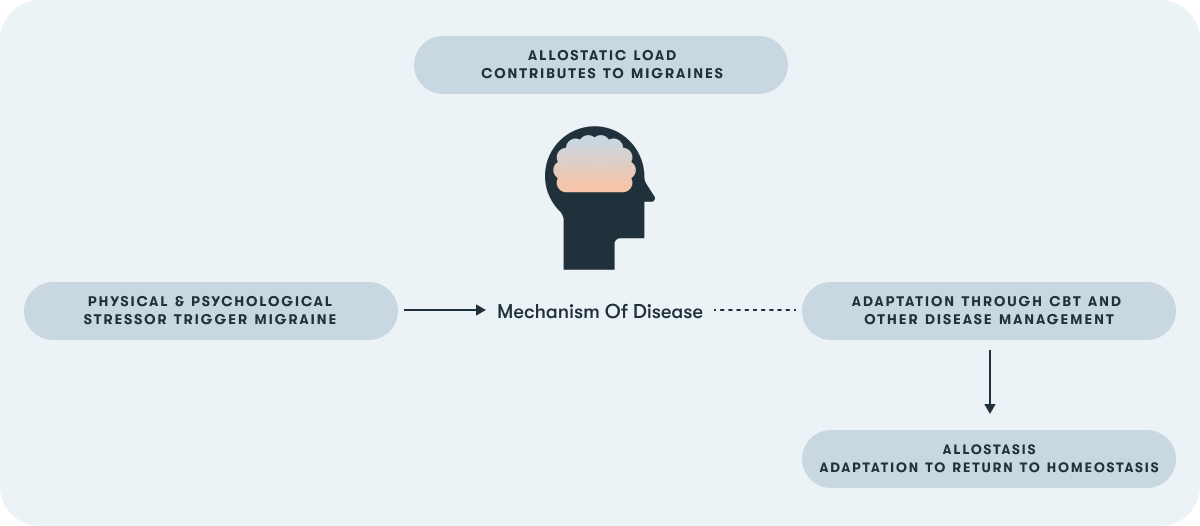
Underlying models conceptualize headache management as strongly influenced by behavioral factors. Treatments are aimed at enabling patients to manage their pain and other associated symptoms more effectively.16 Moreover, the load of stress associated with repeated migraine attacks may contribute to allostatic overload, resulting in a dysregulated neural and endocrine response as previously described in this article.
Managing stress effectively may be crucial to both preventing and managing migraine. Further, depressive and anxious symptoms can be conceptualized as stressors and research has shown that overuse of both migraine and antidepressant medications can exacerbate migraines.17 Thus, it is unsurprising that evidence is mounting that Cognitive Behavioral Therapy (CBT) improves stress management and coping thereby improving the quality of life and functioning of patients with migraine.18
Uses and limits of antidepressants (ADMs)
Currently, the most common way to treat anxiety and depression is prescribing antidepressant medications (ADMs). Most antidepressants target one (or more) of three neurotransmitters in the brain—serotonin, norepinephrine, and dopamine—which are thought to be involved in the pathophysiology of psychological disorders including depression and anxiety.
For example, selective serotonin reuptake inhibitors (SSRIs) block the reabsorption of serotonin; serotonin and norepinephrine reuptake inhibitors (SNRIs) block reabsorption of both serotonin and norepinephrine; and so on. By having higher levels of these neurotransmitters in the brain, it is thought that brain cells can communicate better and mood improves as a result.
Directly targeting the neurotransmitters that are thought to be involved in emotional processing has been described as a “bottom-up” approach to treatment. The medication is theorized to be acting directly on the limbic system (which includes the hippocampus, amygdala, hypothalamus, thalamus, and cingulate gyrus) where emotions are processed, rather than the prefrontal cortex where emotions are regulated.
Despite their widespread utilization, the levels of efficacy for the most common antidepressants are limited for a number of reasons. First, side effects such as sexual dysfunction, weight gain, and sleep disturbance are commonly reported in SSRIs & SNRIs.19 It is true that SSRIs and SNRIs are a newer generation of medications for which side effects are much more tolerable than their predecessors (e.g., tricyclic antidepressants or TCAs), but these newer drugs still cause a number of unpleasant side effects.
But the real issue is that only about 50% of individuals with depression respond partially to medication, and just one third of those on a single antidepressant will achieve remission after 3 months.20 Guidelines suggest taking them for at least 6 months after you start to feel better.21 People who achieve remission but discontinue ADM use are at risk of recurrence at a rate that is 3-5x the risk of a member of the general population experiencing their first episode of depression.22
ADMs also appear to be symptom-suppressive as opposed to curative, and thus many people may need to take medication for several years or indefinitely.23 Moreover, meta-analyses have found that antidepressants are not typically effective for people with mild-to-moderate symptoms.24 But to be clear, these people are still suffering, and they need effective treatments, too.
Finally, up to 30% of depression and anxiety patients do not respond to typical medications prescribed for their disorder.25,26 In the U.S., the Food and Drug Administration (FDA) has approved or authorized other treatments like estkatmine nasal spray and Transcranial Magnetic Stimulation (rTMS) for treatment-resistant depression (i.e., failing two or more trials of medication). The research literature for these treatments is nascent but promising.
In summary, ADMs are not an option for everyone, and those for whom they are effective may experience negative side effects for the duration of their treatment, which could be a lifetime.
Mechanisms of Action and Cognitive Behavioral Therapy's Impact
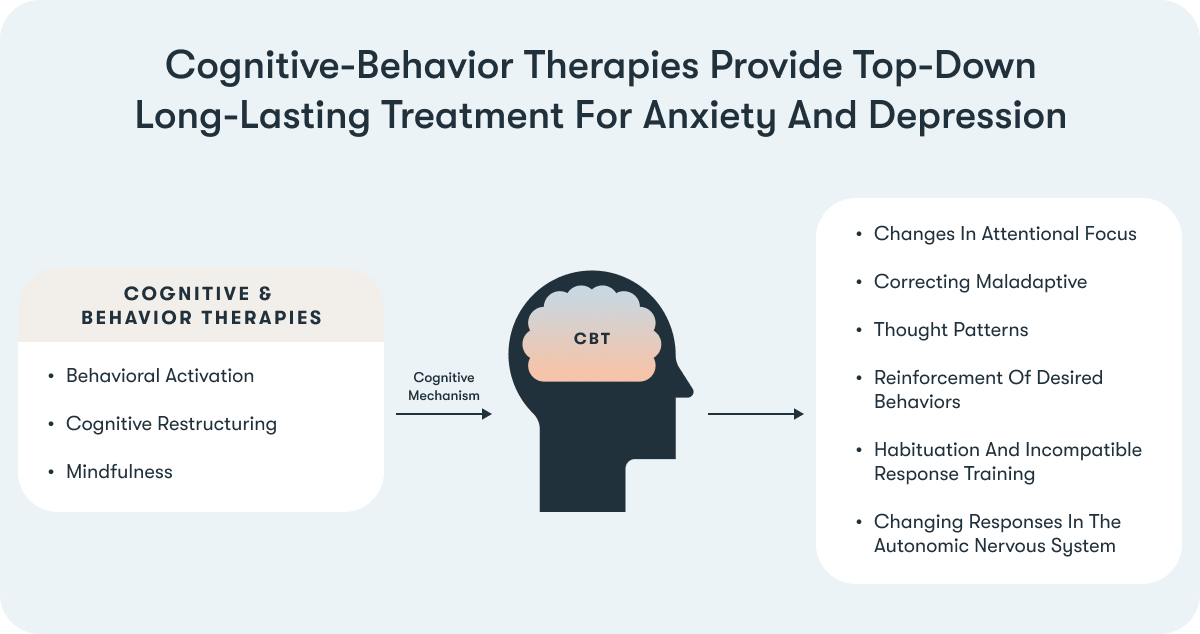
Cognitive Behavioral Therapy (CBT) is an umbrella term for a family of interventions that use at least one behavioral and at least one cognitive intervention. There are many specific and diverse interventions that fall into this category. Some examples include behavioral activation, cognitive restructuring, and mindfulness.
- Behavioral activation helps people to set goals to re-engage and interact with their world in ways they find (or used to find) reinforcing, and are prompted to select an external reward for achieving activation goals (e.g., watching an episode of a favorite TV show after going on a 30-minute walk). Over time, the processes themselves become inherently reinforcing and the external reward is phased out.
- Cognitive restructuring involves identifying thought patterns that are unhelpful and teaches people how to critically evaluate and revise those thought patterns in a way that is accurate and real (i.e., not overly optimistic but not overly emotional, catastrophic, or reactive).
- Mindfulness, or a state of openly observing one’s thoughts, feelings, and sensations without judgement, while not necessarily an intervention in and of itself, has been incorporated into many evidence-based treatments. The basic premise is that being able to observe thoughts while acknowledging that they are just thoughts and not necessarily inherent truths plus the skill of being able to observe and be aware of thoughts and emotional states allows one to reduce distress associated with thoughts/feelings/sensations. It is a central component of Dialectical-Behavior Therapy (DBT), Acceptance and Commitment Therapy (ACT), and Mindfulness-Based Stress Reduction, which all enjoy robust support in the clinical literature.
In CBT treatment, a therapist adhering to program structure recommendations will typically see patients on a weekly basis for 50-minute sessions in either group or individual format (and sometimes both). These sessions tend to be highly structured with review of previous skills and content, review of and troubleshooting associated skills practice homework, followed by the introduction or elaboration of a skill and then planning for the next week’s homework.
A course of CBT therapy varies widely based on the presenting condition(s), but anywhere from 6-20 weeks of sessions is typical. People who completed a course of CBT have demonstrated durable effects that protect against relapse and recurrence, which is not the case for antidepressant medications, likely because CBT teaches skills that can be applied long after the treatment has ended.26
How Cognitive Behavioral Therapy works
While the mechanisms of action for CBT are not well understood, there are some converging findings regarding neural mechanisms as well as many working theories to explain how the different components work. A review of imaging studies found evidence that the resting state activity in the anterior cingulate cortex is reduced after receiving CBT. While previous hypotheses have posited that CBT results in improved efficiency of a “dorsal cognitive circuit” which improves top-down cognitive control and emotion regulation, a review found preliminary signals that this is true, but was unable to definitively conclude that it was accurate.27
With regard to the specific components, it is thought that the cognitive mechanism results in changes in attentional focus and correcting maladaptive thought patterns; behavioral mechanisms include reinforcement of desired behaviors and extinguishing of undesired behaviors, and associative learning; physiological mechanisms include habituation and incompatible response training as well as changing responses in the autonomic nervous system. In an empirical review of meta-analyses of CBT, large effect sizes were found for CBT for unipolar depression, generalized anxiety disorder, and other diagnoses.28
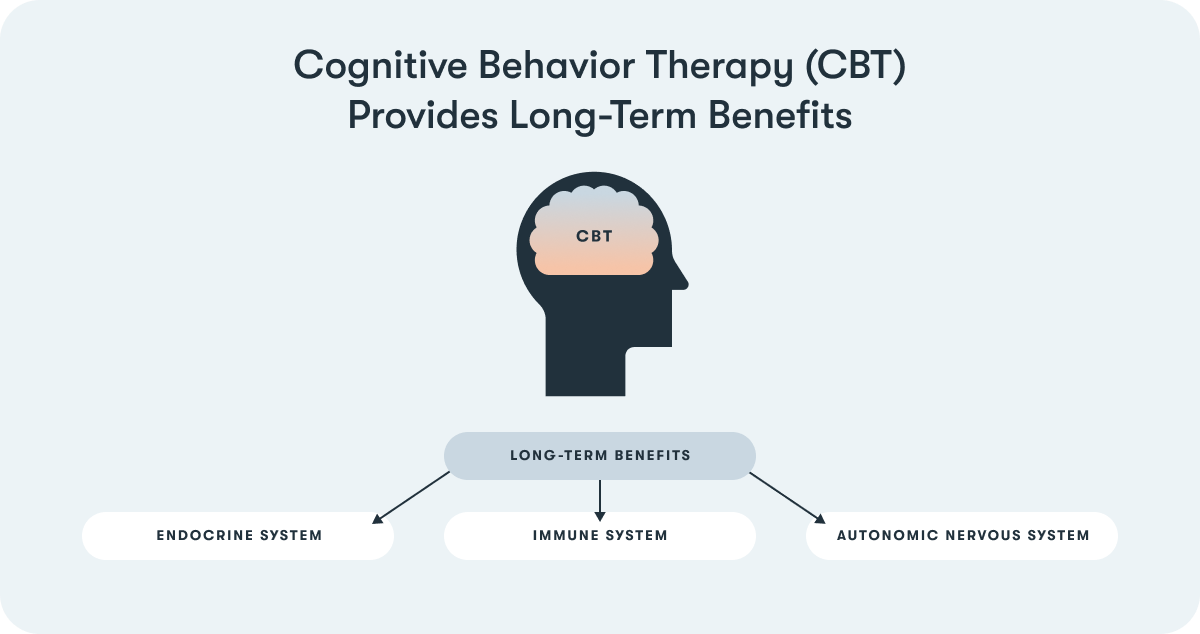
There is considerable evidence to show that CBT has durable effects29, and that it provides long-term benefits despite a relatively brief course of treatment because participants learn skills and tools that they use long after formal treatment ends.30 Research has also found that these kinds of interventions are beneficial to the immune, endocrine, and nervous systems 31, 32, 33
Although the available research concerning the relative effectiveness of CBT as compared to antidepressants appears to be contradictory (i.e., some meta-analyses find better outcomes for ADMs34 compared to CBT, while others find just the opposite35), it is clear that patients have preferences. While certain individuals prefer to take medication to relieve their symptoms, side effects and other aspects of taking medication steer others towards choosing psychotherapy instead. There is also a third group of individuals who decide to attack their problem from multiple angles and receive both (perhaps with added benefit36). Interestingly, a recent meta-analysis found that patients prefer psychotherapy to medication at a rate of 3 to 1.37
Scalability and efficacy of Cognitive Behavioral Therapy delivered digitally
Unfortunately, many mental health practitioners do not provide services consistent with evidence-based treatment recommendations. Therapists who do practice evidence-based treatments are in short supply, typically concentrated in population centers, have long waitlists, and may be difficult to access for logistical reasons.
Fortunately, digital therapeutics (DTx) can deliver cognitive behavioral therapies in a consistent and standardized manner, ensuring that the patient has guaranteed access to a minimum floor of evidence-based care. There are many ways to implement these interventions, and while not a treatment, Twill does so through a combination of games, quizzes, and other interactive activities designed to maximize engagement because even the most effective interventions are not effective if nobody uses them.
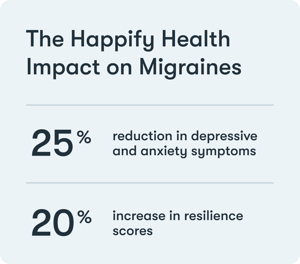 In a randomized controlled trial of Twill, those who used it at least 2 times a week over 16 weeks had an approximately 25% reduction in depressive and anxiety symptoms and a 20% increase in resilience scores, and these improvements were significantly different from the psychoeducation control group. These numbers translate to a net benefit of double the improvement rates over the control group. Moreover, Twill did not just work for those with mild symptoms; in fact those who were highly distressed at baseline improved more from their Twill use.38
In a randomized controlled trial of Twill, those who used it at least 2 times a week over 16 weeks had an approximately 25% reduction in depressive and anxiety symptoms and a 20% increase in resilience scores, and these improvements were significantly different from the psychoeducation control group. These numbers translate to a net benefit of double the improvement rates over the control group. Moreover, Twill did not just work for those with mild symptoms; in fact those who were highly distressed at baseline improved more from their Twill use.38
Digital therapeutics are uniquely positioned to improve whole person health. Their mechanisms of action improve depression, anxiety, stress, health habits and behaviors, and can improve treatment adherence in a way that is engaging and accessible to all. Addressing behavioral and mental health can help to reduce allostatic load, especially for those with chronic diseases or conditions, and improve quality of life and functioning by positively impacting the nervous, immune and endocrine systems.
References
1 Tsigos, Constantine, et al. Stress: endocrine physiology and pathophysiology. Endotext [Internet], 2020 - (link)
2 Sapolsky, Robert M. Why zebras don't get ulcers: The acclaimed guide to stress, stress-related diseases, and coping. Holt paperbacks, 2004
3 Lovallo, William R. Stress and health: Biological and psychological interactions. Sage publications, 2015
4 Chen, Alon, ed. Stress resilience: Molecular and behavioral aspects. Academic Press, 2019
5 Ramsay, Douglas S., and Stephen C. Woods. "Clarifying the roles of homeostasis and allostasis in physiological regulation." Psychological review 121.2 (2014): 225
6 Smelser, Neil J., and Paul B. Baltes, eds. International encyclopedia of the social & behavioral sciences. Vol. 11. Amsterdam: Elsevier, 2001
7 National Alliance on Mental Illness. “Mental Health Facts in America” - (link)
8 Anxiety & Depression Association of America. “Depression” - (link)
9 Anxiety & Depression Association of America. “Understanding Anxiety: Facts & Statistics” - (link)
10 Santomauro, Damian F., et al. "Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic." The Lancet (2021)
11 SingleCare 2020 Drug Report
12 Schwenk, Thomas L. “Comorbid Mental Illness Is Associated with Doubled Healthcare Costs in Patients with Chronic Disease.” NEJM Journal Watch (2019) - (link)
13 Modern Healthcare. “Behavioral Health: Fixing a system in crisis”
14 Deshmukh, Vandana M., et al. "Anxiety, panic and adult asthma: a cognitive-behavioral perspective." Respiratory medicine 101.2 (2007): 194-202
15 Kew, Kayleigh M., et al. "Cognitive behavioural therapy (CBT) for adults and adolescents with asthma." Cochrane Database of Systematic Reviews 9 (2016)
16 Probyn, Katrin, et al. "Non-pharmacological self-management for people living with migraine or tension-type headache: a systematic review including analysis of intervention components." BMJ open 7.8 (2017): e016670
17 Diener, Hans-Christoph, et al. "Medication-overuse headache: risk factors, pathophysiology and management." Nature Reviews Neurology 12.10 (2016): 575-583
18 Dresler, Thomas, et al. "Understanding the nature of psychiatric comorbidity in migraine: a systematic review focused on interactions and treatment implications." The journal of headache and pain 20.1 (2019): 51
19 Ferguson, James M. "SSRI antidepressant medications: adverse effects and tolerability." Primary care companion to the Journal of clinical psychiatry 3.1 (2001): 22
20 Institute for Quality and Efficiency in Health Care. "Depression: How effective are antidepressants." (2015).
21 National Institute for Health and Care Excellence. “Depression in adults: recognition and management.” NICE Guideline CG90 (2009) - (link)
22 DeRubeis, Robert J., Greg J. Siegle, and Steven D. Hollon. "Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms." Nature Reviews Neuroscience 9.10 (2008): 788-796)
23 Hollon, Steven D., Michael E. Thase, and John C. Markowitz. "Treatment and prevention of depression." Psychological Science in the public interest 3.2 (2002): 39-77
24 Fournier, Jay C., et al. "Antidepressant drug effects and depression severity: a patient-level meta-analysis." Jama 303.1 (2010): 47-53
25 Al-Harbi, Khalid Saad. "Treatment-resistant depression: therapeutic trends, challenges, and future directions." Patient preference and adherence 6 (2012): 369
26 Bystritsky, A. "Treatment-resistant anxiety disorders." Molecular psychiatry 11.9 (2006): 805-814
26 Driessen, Ellen, and Steven D. Hollon. "Cognitive behavioral therapy for mood disorders: efficacy, moderators and mediators." Psychiatric Clinics 33.3 (2010): 537-555
27 Franklin, George, Alan J. Carson, and Killian A. Welch. "Cognitive behavioural therapy for depression: systematic review of imaging studies." Acta neuropsychiatrica 28.2 (2016): 61-74
28 Butler, Andrew C., et al. "The empirical status of cognitive-behavioral therapy: a review of meta-analyses." Clinical psychology review 26.1 (2006): 17-31)
29 Wiles, Nicola J., et al. "Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: follow-up of the CoBalT randomised controlled trial." The Lancet Psychiatry 3.2 (2016): 137-144 - (link)
30 Uher, Rudolf, and Barbara Pavlova. "Long-term effects of depression treatment." The Lancet Psychiatry 3.2 (2016): 95-96 - (link)
31 Shields, Grant S., Chandler M. Spahr, and George M. Slavich. "Psychosocial interventions and immune system function: A systematic review and meta-analysis of randomized clinical trials." JAMA psychiatry 77.10 (2020): 1031-1043 - (link)
32 Hammerfald, Karin, et al. "Persistent effects of cognitive-behavioral stress management on cortisol responses to acute stress in healthy subjects—a randomized controlled trial." Psychoneuroendocrinology 31.3 (2006): 333-339
33 Carlson, Linda E., et al. "One year pre–post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients." Brain, behavior, and immunity 21.8 (2007): 1038-1049 - (link)
34 Boschloo, L., Bekhuis, E., Weitz, E. S., Reijnders, M., DeRubeis, R. J., Dimidjian, S., ... & Cuijpers, P. (2019). The symptom‐specific efficacy of antidepressant medication vs. cognitive behavioral therapy in the treatment of depression: Results from an individual patient data meta‐analysis. World Psychiatry, 18(2), 183-191.
35 Li, J. M., Zhang, Y., Su, W. J., Liu, L. L., Gong, H., Peng, W., & Jiang, C. L. (2018). Cognitive behavioral therapy for treatment-resistant depression: A systematic review and meta-analysis. Psychiatry research, 268, 243–250. https://doi.org/10.1016/j.psychres.2018.07.020
36 Dunlop, Boadie W., et al. "Benefits of sequentially adding cognitive-behavioral therapy or antidepressant medication for adults with nonremitting depression." American Journal of Psychiatry 176.4 (2019): 275-286
37 McHugh, R. Kathryn, et al. "Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review." The Journal of clinical psychiatry 74.6 (2013): 0-0)
38 Parks, Acacia C., et al. "Testing a scalable web and smartphone based intervention to improve depression, anxiety, and resilience: A randomized controlled trial." International Journal of Wellbeing 8.2 (2018)
About the Author
Alyssa Dietz, Ph.D. and Chris Wasden
